
Major study offers practical guidance on antibiotic dosing in patients with obesity
Leiden researcher Anne-Grete Märtson brought together a large number of studies to better understand antibiotic dosing in patients with obesity. The publication in a renowned medical journal has already garnered much positive reactions, Märtson says. ‘It’s high time researchers started sharing more data.’
Before she was a researcher, Anne-Grete Märtson joined doctors on their ward rounds at a hospital in her native Estonia. ‘As a clinical pharmacist, I focused on the medication: was a certain combination of drugs safe, what was the optimal dose? I also monitored for potential liver and kidney damage caused by different medications.’
The infection may worsen for some patients
A growing challenge for doctors and pharmacists is the rising number of patients with severe obesity. Märtson explains: ‘We’re increasingly seeing limited responses to administered medicines – in some patients the infection even worsens. Medicine package insert doesn’t provide dosing guidance for people with obesity.’
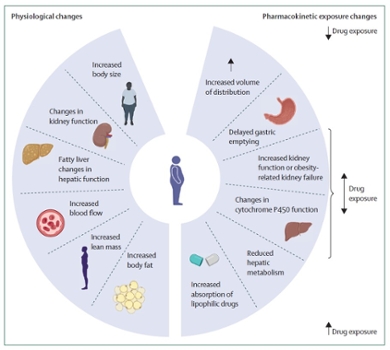
Antibiotics, which fight bacterial infections, pose an additional challenge. ‘If the dose is too low, some resistant bacteria can survive, increasing the risk for the drug to not work anymore.’ With certain medicines, you can easily adjust the dose based on body weight, but that’s far from always the case. For instance, in people with fatty liver – a condition more common in those with obesity – there’s a higher risk of overdosing, as the drug is broken down more slowly.
128 studies analysed
Märtson led an international team of renowned researchers to compile what is currently known about optimal antibiotic dosing in people with obesity. ‘We reviewed the abstracts of over 4,000 studies in this field and identified 128 that were relevant enough for in-depth analysis.’
The drug behaves differently
They found that common antibiotics – those used in hospitals and GP practices for conditions like pneumonia or bladder infections – behave differently in people with obesity. ‘They distribute differently across the body’s tissues. Sometimes too little reaches the lungs, even though you’re trying to treat a lung infection.’ Still, Märtson does not recommend to simply increase the dose. ‘In critically ill patients, it can be helpful to administer the dose over two to four hours instead of half an hour via infusion.’ The goal is to achieve optimal blood concentration of the antibiotic. ‘It’s important that the concentration is monitored.’
For another class of antibiotics, aminoglycosides, such monitoring is standard practice, as overdosing can cause kidney and irreversible hearing damage. ‘For this type of antibiotic, a specific calculation based on body weight can guide a safe dose increase.’
Modern techniques offer great potential
Clinicians have responded positively to the findings, though the team also concluded that for many antibiotics, there is still too little data to make strong recommendations. Märtson: ‘There are excellent methods available to conduct high-quality research into this issue. Using large databases and predictive models, we can make great strides. A CT scan, for instance, can assess body composition in trial participants. We came across many small-scale studies. I hope researchers will start sharing more data, so we can ultimately establish proper guidelines for all antibiotics.’
