
New zebrafish study to understand human cancer
Ewa Snaar-Jagalska, Shuning He and colleagues from IBL, LION and LACDR reported on a new zebrafish study to understand micrometastasis of human cancer cells. They discovered a novel role for neutrophils in assisting metastasis formation, which provides critical insights for anti-cancer therapies.
In a recent issue of the Journal of Pathology, Ewa Snaar-Jagalska, Shuning He and colleagues from IBL, LION and LACDR described zebrafish as a model system to study micrometastasis of human cancer cells and discovered a novel role for neutrophils in assisting metastasis formation. They also show how this behavior of neutrophils may interfere with common anti-cancer therapies.
How cancer cells establish metastasis and respond to therapy are fundamental questions in cancer research. The engraftment of fluorescent tumor cells into zebrafish embryos with fluorescent blood vessels and immune cells is a powerful system for studying the role of the tumor microenvironment during metastasis formation. By non-invasive, high resolution imaging of the whole living animal with developing cancer we discovered that the physiological migration of neutrophils controlled tumor invasion by conditioning the collagen matrix and forming the metastatic niche. Simplifying, immune cells prepare the soil (i.e. the metastatic niche), where tumor cells can seed and form metastasis.
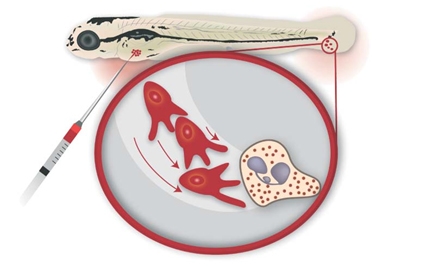
The findings of Snaar-Jagalska and colleagues may have important implication for anti-cancer therapies that target the vascular endothelial growth factor receptor (VEGFR) to block tumor angiogenesis. Such therapies proved very effective in reducing local tumor growth, but increased metastasis in some patients has been reported as a dangerous side effect. In the zebrafish model, administration of VEGFR inhibitors was found to enhance migration of neutrophils, which in turn promotes tumor cell invasion and formation of metastasis. This unexpected result demonstrates the in vivo cooperativeness between VEGF signaling and immune cells in metastasis and provides a new mechanism underlying the recent clinical finding that VEGFR targeting can promote tumor invasion.
There is clearly much work needed to understand the role of neutrophils and anti-VEGF therapies in cancer biology. Future use of our zebrafish model, now the accepted by a medical Journal, can make a great contribution to further enhance our understanding of how immune suppression and targeted therapies function at the whole animal system level.
Links
- Neutrophil-mediated experimental metastasis is enhanced by VEGFR inhibition in a zebrafish xenograft model, Shuning He1, Gerda E.M. Lamers1, Jan-Willem M. Beenakker2, Chao Cui1, Veerander P.S. Ghotra3, Erik H.J. Danen3, Annemarie H. Meijer1, Herman P. Spaink1 and B. Ewa Snaar-Jagalska1 (1: Institute of Biology, 2: Leiden Institute of Physics, 3: Division of Toxicology, Leiden Academic Center for Drug Research, Leiden University), http://onlinelibrary.wiley.com/doi/10.1002/path.4013/pdf
- Commentary paper in Journal of Pathology: Live imaging in zebrafish reveals neu(trophil) insight into the metastatic niche, E. Elizabeth Patton, http://onlinelibrary.wiley.com/doi/10.1002/path.4051/pdf
- Web page of ZF-Cancer project
