Skin Barrier and Vaccination
Research lines
Current research at the Skin Barrier and Vaccination group.
Intradermal vaccination by means of microneedles
Microneedles are needle-like structures with a length of maximal 1 mm and a diameter in the mm range. In our group microneedles are used either as a single hollow microneedle or as solid microneedle arrays. As microneedles are short and the skin is a very elastic, reproducibly piercing into the skin is a challenge. To achieve this goal various impact-insertion applicators have been developed. Hollow microneedles are predominantly used to test (nanoparticulate) formulations on their efficacy to induce an immune response. As the physical properties of the nanoparticles may affect the immune responses, the particles are thoroughly characterized. The size distribution of nanoparticles is measured by dynamic light scattering and nanoparticle tracking analysis. Encapsulation of protein is analysed by ELISA or fluorescence spectroscopy. The stability of the proteins in formulations is measured by UV spectroscopy, flow imaging microscopy and asymmetrical flow-field fractionation.
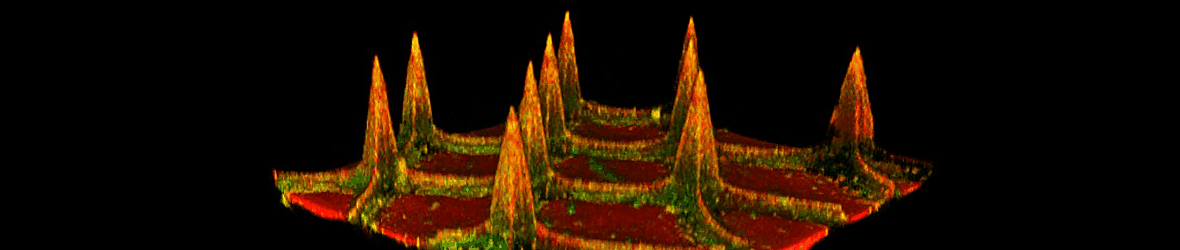
Besides the hollow microneedles, we also have developed coated and dissolvable microneedles. Coated microneedles are prepared using pH sensitive silicon surfaces on which alternatingly positively and negatively charged material are applied resulting in multilayers of antigen and polymer or adjuvant, see figure 1. Dissolvable microneedles have been developed with hyaluronic acid as matrix material. Both types of solid microneedles are also combined with antigens encapsulated in nanoparticles. Microneedles with the (encapsulated) biologics are thoroughly characterized with respect to skin piercing efficiency and the delivered antigen dose in the skin. The latter is performed by in vivo infrared-imaging analyser. (Model) antigens that have been explored are diphtheria toxoid, ovalbumin, synthetic long peptides and inactivated polio vaccine. Recently a new project was initiated in which microneedles are developed for tuberculose vaccination.
Impaired skin barrier of inflammatory skin diseases
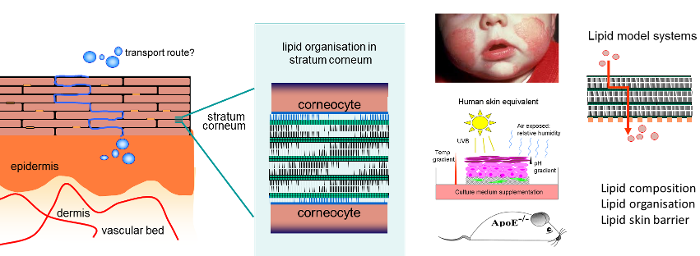
Among the various inflammatory skin diseases, atopic dermatitis is the most prevalent one. Atopic dermatitis is a chronic inflammatory skin disease often associated with asthma. It has been related to factors such as detergents and the appearance of dust mites on the skin surface and a dry environment. Although for many years it has been reported that allergens initiate the disease, in recent years it has become clear that in a subpopulation of the patients the disease is triggered by an impaired barrier function of the skin, which facilitates the transport of allergens across the stratum corneum. Due to this facilitated transport there is a high risk for the formation of eczematous lesions.
Our research focus is to examine the role the barrier lipids in atopic dermatitis, but also in other inflammatory diseases such as psoriasis and netherton syndrome. The main lipid classes are ceramides, free fatty acids and cholesterol. The lipid composition and organisation in the stratum corneum of atopic dermatitis patients were assessed. An excellent correlation was observed between several of the lipid properties and a reduced skin barrier emphasizing that indeed lipids play a prominent role in the impaired skin barrier function in these patients. Techniques used are mass spectrometry, Fourier transform infrared spectroscopy, Raman spectroscopy and small- and wide-angle X-ray diffraction (Synchrotron facilities Grenoble).
These observations resulted in various follow up studies:
- We examine whether inflammation indeed may affect the lipid properties in the skin barrier by supplementation of cytokines to the culture medium during generation of three-dimensional human skin equivalents (see figure 2). Our studies show that inflammation affects the lipid composition in stratum corneum of cultured skin similarly as observed in atopic dermatitis patients. In addition we also examine the expression and activity of enzymes involved in ceramide and fatty acid synthesis and how this changes in inflamed skin.
- Using lipid model systems (see figure 2), in which we link information on lipid organisation and lipid composition with skin lipid barrier properties, we study whether the changes observed in the lipid composition in inflamed skin results in a higher flux of compounds through the lipid matrix.
- One of the possibilities to reduce the chance for eczematous regions, is to repair the barrier function of non-lesional skin by supplementation with those lipids that are present in reduced quantities in the stratum corneum lipid matrix. Ex vivo and in vivo (clinical) skin barrier repair studies are performed in which formulations are topically applied on a impaired skin barrier, The composition of the formulations is based on vernix caseosa.
- Related to these studies we also examine whether there is a co-morbidity between atherosclerosis and inflammatory skin diseases. Here we make use of atherosclerosis mice models and investigate whether selected knock-out models (altered distribution in lipoproteins fraction towards HDL or LDL and VLDL) result in a change in the barrier lipid properties and may induce skin inflammation.
Strongly related to the above research themes are two other projects: 1) A detailed analysis of the lipid organisation of the two lamellar phases detected in the stratum corneum. The localisation and conformation of the barrier lipids assembled in these lamellar phases are assessed by a combination of neutron diffraction (neutron sources: ILL at Grenoble and ISIS at Rutherford Appleton Laboratory, Harwell Oxford), X-ray diffraction (ESRF synchrotron facilities, Grenoble) and Fourier transform infrared spectroscopy. These studies are of eminent importance for understanding how changes in lipid composition affect the lipid organisation and thereby the skin lipid barrier and 2) The develop a new generation of reproducible human skin equivalents that mimic all barrier properties of native human skin. When analyzing the barrier function of human skin equivalents in details, it appeared that it deviate substantially from human native skin. By supplementation of compounds to the culture medium and by mimicking the culture environment that more closely the natural skin environment we aim to normalise the skin barrier by normalising the lipid properties in the stratum corneum.