
How e-coaching helps people with chronic kidney disease to live more healthily
An e-coaching programme helps people with chronic kidney disease, particularly in areas that patients themselves want to work on. ‘A healthy lifestyle is important for patients with kidney disease: it can slow down the loss of kidney function and there will be fewer complications,’ Katja Cardol explains about her research on lifestyle and self-management. PhD defence 16 March.
Around a quarter to a third of people with chronic kidney disease have psychological symptoms, such as anxiety or depression. Health psychologist Katja Cardol explains: ‘We thought, based on prior research, that these symptoms made it difficult to have a healthy lifestyle, so we developed an online programme for people with kidney disease to help them live more healthily and learn to manage their condition. People have to be able to deal with their diagnosis, a future that may look different from what they were expecting, unwelcome symptoms and maybe also social change.’ That’s a lot to have to cope with, and it is logical that they will have psychological difficulties. We investigated whether that was in fact the case, and whether it helps if you offer them treatment on how to manage their condition.’
E-coach Cardol
‘What I really liked about this PhD track was setting up the study and the contact with patients in four hospitals spread throughout the country: the LUMC and HMC Haaglanden in The Hague, University Medical Centre Groningen and Radboud University Medical Centre in Nijmegen. It was very satisfying to be close to the actual people with chronic kidney disease as a healthcare provider, because in my role as a psychologist or e-coach I had the opportunity to treat some of the patients personally.’
Getting to work on your own goals
‘What I really liked about this PhD track was setting up the study and the contact with patients in four hospitals spread throughout the country: the LUMC and HMC Haaglanden in The Hague, University Medical Centre Groningen and Radboud University Medical Centre in Nijmegen. It was very satisfying to be close to the actual people with chronic kidney disease as a healthcare provider, because in my role as a psychologist or e-coach I had the opportunity to treat some of the patients personally.’

What was already going well
‘An exercise on strengths and resources of support was popular among the participants. In the exercise, we asked about a person’s strong points, and times when things were going well in terms of living healthily. What helped them at those times? How can other people support you? We asked them to talk to different people about it, asking them things like: ‘What do you think my strengths are?’ That gave their motivation and self-confidence a boost. Things that are already going well are nice, and you can work on strengthening them even further to make a healthy lifestyle easier.’
No one size fits all
‘Some of the participants with psychological distress indicated that they wanted to make changes because these complaints were hampering them in their lifestyle behaviours. But there are other obstacles, too. Some people find it difficult to change their behaviour because they have very little social support, and others don’t really know what is healthy and what isn’t. One person wants to be more active, and another wants to quit smoking. Everyone has different issues and different resources. Our research showed that not everyone experienced reduced psychological complaints after treatment. That’s actually logical because each participant had personal treatment goals for their particularly relevant problems and lifestyle behaviors.'
Personalised approach works well
'We did see progress on a personalised outcome measure, which measures progress on an individual’s own priorities. Given that everyone was working on different issues, we also needed to measure whether they improved in those self-selected areas. The effects we didn't find are also very relevant. Just the combination; you might see that general measures like psychological distress or quality of life do not improve, whereas personalised measures do. This contrast also prompted us to ask the question: 'Hey, maybe we should use a different method of measuring effects in research on person-centred care. Not just tailored treatment, but also tailored outcomes.'
Innovative
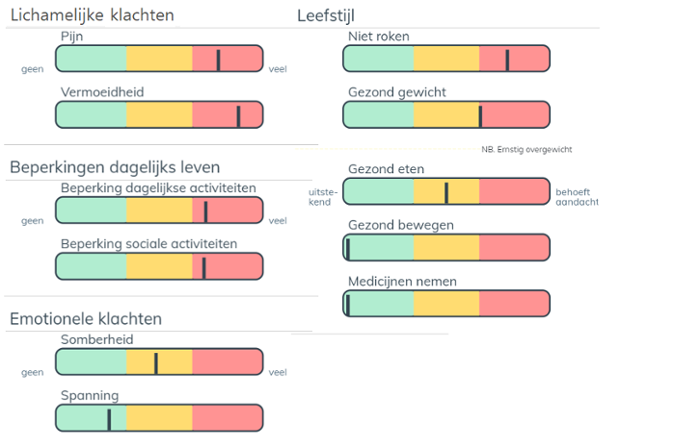
'With this insight, we developed our own Personalised Priority and Progress Questionnaire, based on existing personalised instruments, which reflects truly personally meaningful outcomes. We also conducted a validation study, to check whether the questionnaire is valid and reliable. In the future, we can tailor and explore the personalised instrument further for different target groups. What’s also innovative is the digital screening tool in which we offered the questionnaires. It shows patients a graphic representation of their well-being and lifestyle: the Personal Profile Chart, with a kind of traffic light model. This allows patients and their caregivers to immediately see what is already going well and where gains can be made with follow-up steps that fit each patient's personal needs.'
Being chronically sick is like being a top athlete.
Just like a professional athlete
‘In addition to teaching psychology students and healthcare professionals, I want to expand my own business as a sport and health psychologist. Working with athletes has a lot of overlap with health and medical psychology because you are often working on athletes’ lifestyle and energy balance. How do you recover, what helps you to recharge your own batteries, and what things drain your energy? These are the same issues I discuss with people who have a chronic illness. Being chronically ill is in some ways pretty much like being a top athlete. You can also think of the high level of pressure that healthcare professionals experience: how do you perform optimally and maintain a healthy work-life balance? As a Sport & Health psychologist, I combine both: the medical and the sports worlds.
